
Meeting my TGA baby | Pumping | Balloon Septostomy #CHDawareness
As Leyton’s first birthday rapidly approaches, I’ve been reflecting a lot on all he’s overcome in the last year. I recently shared a blog post about receiving our baby’s TGA diagnosis, a Congenital Heart Defect (CHD) here and his birth story here, but there is so much more to his story.
Over the next few weeks I’ll be diving into the archives and chronically the wild ride that made up our warrior boy’s first month of life.
*I wrote the following intro 3 months post-op, so please forgive all the time hopping.
This week marked 3 months since Leyton’s open heart surgery. It honestly feels like 3 years ago and I’m not sure if that’s because newborn life is all-consuming and rapidly changing or because I buried the memories that are difficult to relive. Either way they still pop up from time to time, often when I least expect it.
I was sitting at the DMV recently (which is always such a lovely way to pass the time 🙃) and the man seated next to me started drumming his fingers on his plastic chair. It sounded exactly like the blood pressure cuff that squeezed Leyton’s calf multiple times per hour when we were at CHLA. He absolutely hated it.
My body stiffened and my stomach shot into my throat – a visceral response to the sound and the memories attached to it. I instantly relived the helpless feeling of attempting to console my baby and keep him still long enough to get an accurate reading, knowing if I couldn’t then the whole process would start over again. It was torture seeing our newborn upset amongst all the wires and IV’s. Much of the time he wasn’t able to eat, let alone breastfeed, so our comfort measures were limited.
My dramatic response to a stranger’s finger drumming highlighted that I just *might* still have some processing to do, and urged me to write it all out. I have notes in my phone with bullet points of what happened in the hospital each day, and I always intended to write it down in greater detail. I found it comforting to read other TGA and other CHD stories on Instagram when I was pregnant and terrified of what was to come. Now I’m ready to share our honest story of Leyton’s first few weeks of life; the good, the miraculous, and the ugly.
Leyton was born at 10:45pm (you can read my labor and delivery story here if you want to start at the beginning) and taken straight up to the NICU so they could evaluate his heart and begin around the clock monitoring. Before we was born the hospital asked for our signed consent to place an umbilical line and quickly administer prostaglandin, a medication used to keep the opening between the aorta and pulmonary arteries open. If this opening (called the ductus arteriosus) closed as it normally does shortly after birth, then oxygenated blood wouldn’t be able to circulate his body or reach his brain. It’s critical that TGA babies receive this shortly after birth, which is one of the greatest advantages we earned when he was diagnosed prenatally.

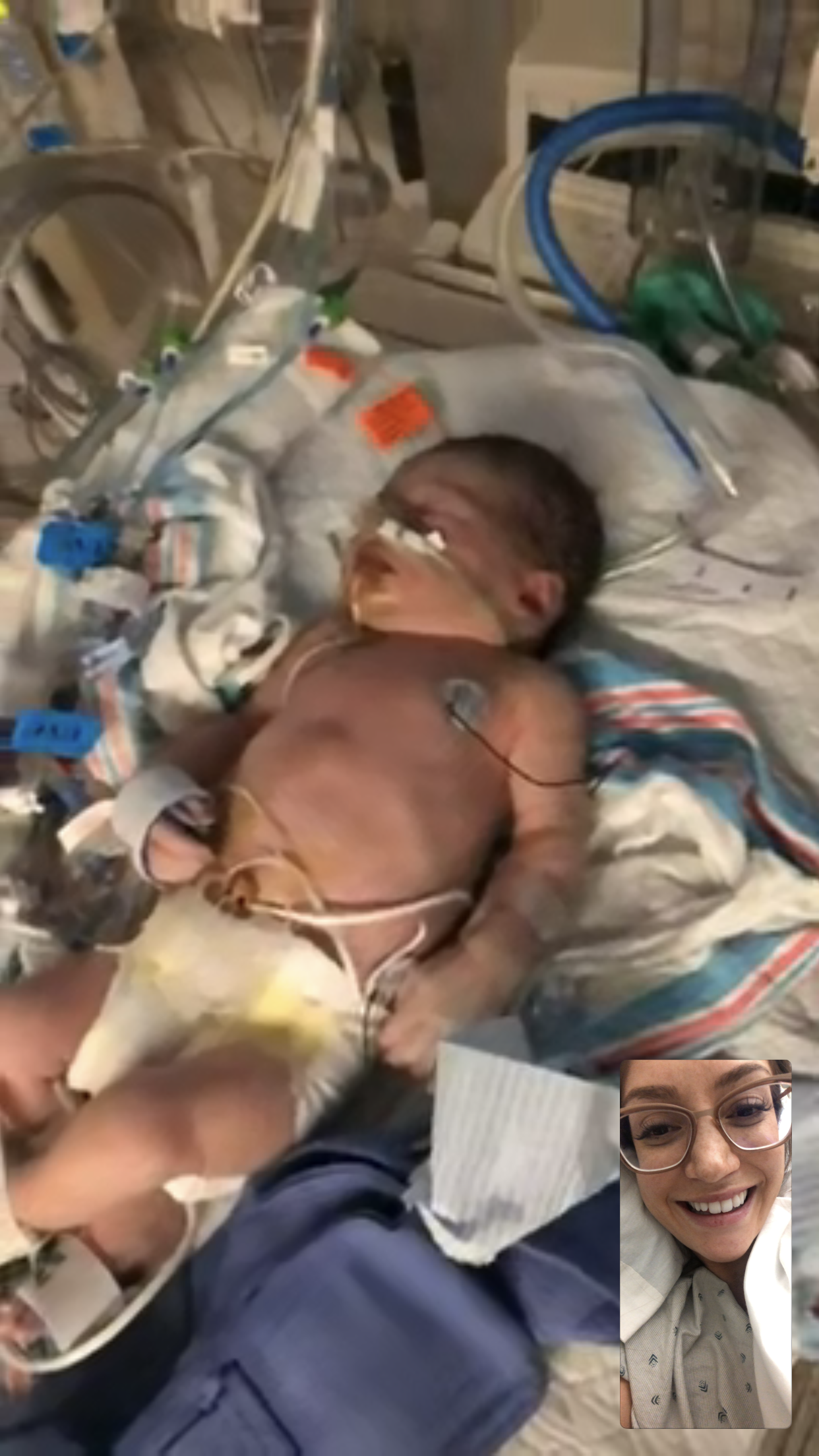
Jordan went up to the NICU to visit Leyton several times in those early hours and FaceTimed me so I could see him too. He was stable and at that point his condition was more or less what we expected it to be. As desperate as I was to hold or even see my baby, I felt a bit more at ease knowing he was getting the care he needed and should anything change, he had an entire team there for him.
Around 3am, after one of our FaceTime sessions it occurred to me that I had no clue how to use the Medela breast pump that sat next to me for hours. I knew it was important to start pumping shortly after birth since he wouldn’t be able to breastfeed for a few days (it ended up being a few weeks, but we’ll get to that eventually 😭). I rang for the nurse who patiently walked me through my first pump session.
Pumping was an act only I could do for my baby in that moment and I felt so proud. The nurses wanted me to wait until morning to go see him because I was still weak from delivery, so pumping gave me something to do other than long to be with him!
My mom and Jordan came back to my room after visiting Leyton and set up their sleeping arrangements. My mom tried and failed to sleep in the waiting room (which was no surprise between the blaring lights and families gathering) so the three of us had a slumber party in my recovery room.
I’ll never forget the sight of the two of them sleeping (they looked so uncomfortable 😭) while I sat up in my hospital bed excitedly pumping away in the middle of the night. I was able to pump half an ounce of colostrum, which the nurse seemed pleased with. I dozed off for the first time in almost 24 hours until the NICU called to say Leyton needed a balloon septostomy procedure and Dr. Zahn would be there shortly to perform it.

We were prepared that he might need this procedure as many babies with TGA require it shortly after birth, but there was no way to tell for sure until he was born. His oxygen levels were dropping and he was having trouble breathing, so they couldn’t afford to wait any longer.
A balloon atrial septostomy is when a catheter with a balloon on the end is inserted through a vein in the baby’s groin. The balloon is then inflated and used to expand the foramen ovale or atrial septal defect (essentially a hole in the heart) to allow for more blood to mix together. Before a TGA baby can undergo open heart surgery, the best way to improve oxygen levels is to allow oxygenated and deoxygenated blood to mix.
I called at 6am hoping to see him before the procedure started, but the nurse told me they were already prepping him so I couldn’t go. I pumped again and then my sister arrived. She booked a flight to LA from Portland as soon as I told her I was in labor and she arrived just hours after Leyton was born! She and my mom stayed with us for weeks after Leyton’s surgery. <3

Dr. Zahn and Dr. Markush, Leyton’s interventionist and cardiologist, came down after the procedure. They said everything went well although it was a bit trickier than anticipated due to the anatomy of his heart. However, I heard approximately 0% of anything they said after they let me know I could finally go see him. I would have sprinted up there myself if it wasn’t hospital policy to transport me in a wheelchair.


Finally I laid eyes on my baby 12 hours after birth. I wasn’t able to hold him, but I reached into the isolette and squeezed his little hand and rubbed his tiny feet. He was quite sedated, but I was comforted knowing on some level he knew we were there with him. I remember thinking he looked so healthy in the moment, but now knowing what his true coloring is I can see the effects of his low oxygen levels, a common side effect for babies with TGA and other CHD’s before they’re repaired.


Gradually throughout the day the magical glow of Leyton’s safe arrival became overshadowed by the reality of what he, and we, were facing. The reports of his condition painted a less optimistic picture with each visit and during my final trip to the NICU that evening I saw him cry for the first time. I use the word “saw” because he was intubated so his cry wasn’t audible.
Seeing his pained expression as he let out a silent cry was one of the most helpless feelings I’d ever experienced. I was alone at the bedside and just sat there and sobbed with him. It’s a moment I’ll never forget. I remember thinking, “No mother should have to experience this. Ever.”
His condition continued to become more unstable as the night waned on, and we woke up to a clearly stressed and focused report from his nurse the next morning. Things started to move quickly then, so I’ll save the events of the days that followed for my next post.

