
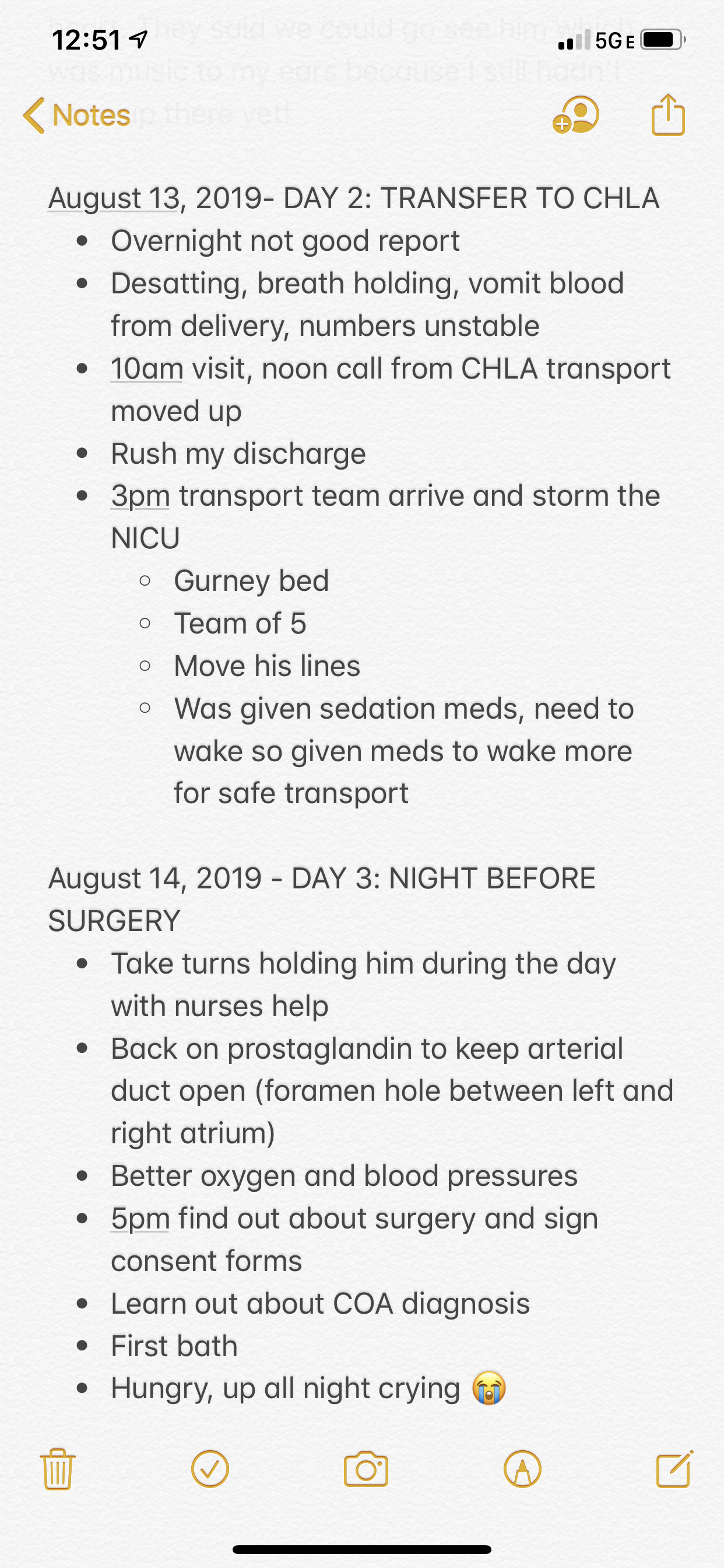
CHLA transport | New diagnosis | The hardest night yet…
When I last left off, Leyton was 2 days old and still in the NICU at Cedars Sinai where he was born. We knew he’d eventually be transported a few miles away to Children’s Hospital Los Angeles to undergo surgery to repair his heart. Timing the transport was tricky because I was still a patient as well, so we hoped I’d be discharged before him to avoid separating us.
Leyton was born late at night, so I was expected to spend two nights in the hospital. The great thing about moving him to CHLA was that both Jordan and I could stay with him in the room 24/7, a luxury we didn’t have while he was in the NICU.
The teams at both hospitals were in constant communication. CHLA received regular updates on Leyton’s condition and prepared for his arrival. They were supposed to notify us when a room was available, but it was expected to be later that week.
Jordan and I fell into a rhythm for our Leyton visits. We followed our favorite route from my room to the NICU, checked in, stopped to scrub in, and greeted his nurses at the bedside for a report. Our morning report that day was concerning. He had several episodes overnight; holding his breath, vomiting blood, and desatting (unstable or low oxygen levels) keeping the nurses “on their toes” as they put it, all night long. My poor baby.
We stood with him for a while, but eventually I had to go back to the room to rest. I had a small tear and a few stitches from delivery so even though I managed the pain with Tylenol, my body still felt incredibly weak. I remember being surprised, naively thinking a natural delivery meant I might be spared from typical postpartum recovery. 😉
We returned an hour later and learned that CHLA was concerned about Leyton’s status and moved up his transport. They were on their way to get him…ASAP. We were surprised, but sprang into action. Jordan ran downstairs to speak to my nurses about discharge (aka he announced that I was leaving LOL), I rushed to fill out the birth certificate, and my mom and sister helped pack up my room.
Transport
The next thing I knew a team dressed in black pushing a giant gurney with an isolette perched on top rounded the corner. I smiled and one of them said, “Mom?” I nodded and showed them over to Leyton. That wasn’t the first or last time I was addressed as Mom in the hospital but it never got old and I was always happy to hear it. 🙂

If you read the screenshot above (they’re the unedited notes I jotted down in the hospital, hence the spelling and grammatical errors) I wrote the team, “stormed the NICU”. That’s exactly how it felt! It was a whirlwind of commotion and everything happened so fast. The whole scene felt very dramatic. Jordan and I were in awe of how efficiently the team worked. They took immediate control and we trusted them instantly.
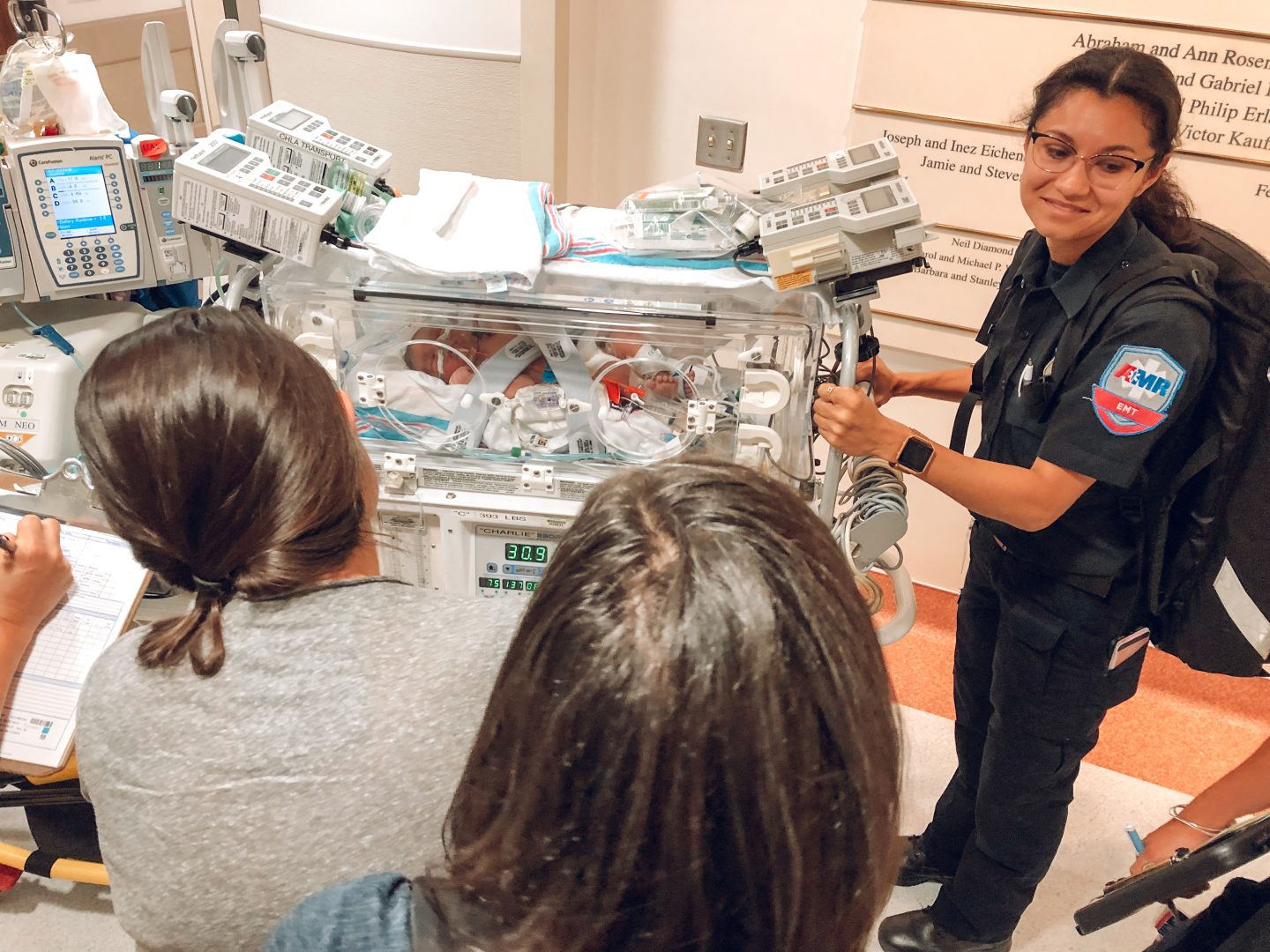
Unfortunately, Leyton had just received a dose of sedatives and they weren’t comfortable transporting him in his current condition. They administered another medication to “wake him up” a bit.
This was one of the many moments I mourned the life I always imagined for my son. One where snuggles and breastmilk could heal his every ailment. Yet instead, doctors pricked and injected my newborn with more medication than the average adult receives in a lifetime. Logically I knew these measures were not only necessary, but life saving, however that wasn’t enough to soften the hit to my mama heart.
After they transferred all his lines and hooked him up to the portable machines, we booked it for the transport vehicle. Honestly, looking back I don’t know how I did it. I was 36 hours post-delivery and unable to sit comfortably without bleeding profusely (I know moms who delivered remember just how glamorous those early postpartum days are) and here I was r u n n i n g through the halls of the hospital. The step into the ambulance cabin was at least 2 ft high, and I remember hoisting myself up and just praying I didn’t pass out or rip a stitch. With that said, I was so happy to be there with my baby, I would’ve done cartwheels down the hallway if that’s what it took!

We weaved our way through LA rush hour traffic with the sirens blaring and made it to CHLA in 12 minutes. Jordan and my family followed, but it took them quite a bit longer to get there.
Checking into the CTICU
The commotion in the NICU was nothing compared to the scene waiting for us in his new room. I struggled to find my bearings as 15 medical professionals hovered around Leyton. They all worked simultaneously, and all I could think was, how on earth are they able to think clearly, let alone communicate? It’s their norm but it felt like pure chaos to me.

I must’ve looked like a child quietly sitting there with my hands in my lap, feeling helpless and overwhelmed. A friendly face approached me with mile long lashes and a huge smile. Carley, the charge nurse, introduced herself and reassured me that everything was going to be ok. She handed me a form to fill out with some painfully basic questions (what language do you speak at home, who lives in your household, etc.) yet in my daze it took me 10 minutes to fill out.
Finally Jordan arrived and the doctors and nurses slowly trickled out of the room. I breathed a sigh of relief and took in our surroundings for the first time in hours. Our room was large and private, although we shared a bathroom with the patient next door. Leyton looked so tiny in his isolette in the middle of the room, flanked by a dozen machines and tanks on either side. We brought a few pictures and other items from home to add a personal touch to the room.

We spent the rest of the evening taking turns holding him. It was the first time for me, Jordan and our parents! The nurse let us help her give him his first bath. It was a bit unorthodox given right in his isolette, but a momentous occasion nonetheless! I cherished all the “firsts” as special moments and pushed through the emotions surrounding how unique they were. In some ways, we were able to extend the newborn phase and got a second round of “firsts” when we got home.


The next day we continued holding him for hours at a time. He was always calm in our arms. So much so, that his heart rate would dip at times and we’d have to jostle him awake a bit.
A New Diagnosis
His surgeon operated on Mondays and Thursdays, so we were prepared to wait through the weekend and have his surgery the following Monday. Except that afternoon the doctors informed us they would be operating the next day at 8am.
By that point, we were numb to these surprises and the lingering feeling of uncertainty. We expected the unexpected, however it was unsettling having merely a rough outline of the events to come. An exact timeline and the details of our baby’s wellbeing were always a huge question mark. I still struggle with these feelings today, so I can’t say that part gets any easier.
The doctor handed us a digital consent form on an iPad to sign. I scrolled past the part on risks of surgery, including death, with a lump in my throat wishing once again that I could scoop him up and run away.
About twenty minutes later, the doctor returned and explained that after looking carefully at his echocardiogram (an ultrasound of his heart) he discovered an additional heart defect that they hadn’t detected previously, called Coarctation of the Aorta.
We were still reeling from his new and sudden surgery date, so another diagnosis and additional complications felt like a massive blow. We signed the new consent form that reflected the second operation and went to bed feeling heavy.
I set alarms and woke up every 3 hours to pump, but they weren’t necessary that night because Leyton cried all night long. He dozed off for a few minutes and then woke up screaming over and over. The nurse rushed in and we took turns trying to comfort him until he settled, but it was always short lived. My heart broke for him and I can’t even describe how long that night was. I reached a new level of exhaustion so all-consuming, every fiber of my body hurt.
Leyton hadn’t received any nutrition other than clear fluids and had to continue fasting before surgery, so not only was he irritable from all the meds, he was starving too. Finally by 5am I asked the nurse if I could try holding him. He instantly fell asleep in my arms, and we sat in that chair for the next 3 hours until they came to prep him for surgery.


I sobbed and apologized to him over and over, wiping my tears off his forehead. The night was horrific, but I felt an ounce of comfort in the few hours of peace he received before surgery.
I’ll share the rollercoaster of events that took place during and after his surgery in my next post. As any heart parent will tell you, it was the longest day of our lives.

