Heart Month continues! We’re in the home stretch, but I have so much still to add to my CHD series for heart parents. Today’s post is all about preparing for surgery, recovery and life in the hospital after your child’s open heart surgery. If you’re new to Heart Month, feel free to start here.
Prepping in Pregnancy
It is clinically proven that a prenatal CHD diagnosis can lead to better outcomes. It allows the baby’s medical team and parents to put a plan together for immediate critical care. However, receiving my son’s TGA diagnosis also added a daunting layer of stress to my final months of pregnancy.
My third trimester was marked by weekly appointments with specialists. Every answer I received about Leyton’s condition seemed to lead to 3 new questions. I remember being completely overwhelmed some days and blissfully excited to meet my baby the next. It was a roller coaster. But the roller coaster really kicked into high gear once he was born, so I’m so glad I was able to use some of my pregnancy to prepare for his surgery and recovery.
I learned so much about TGA during that time. I found other heart moms on social media and read their stories. My YouTube library was full of birth vlogs and hospital bag videos. Learning as much as possible became a coping mechanism for me.

Honestly though, I cried a lot too, and felt like I went through every emotion under the sun! I tried my best to ride the wave of each emotion as it came. Thanks to an amazing support system, I never felt like I had to bottle it up. Unconsciously I think this helped prepare me for his surgery and the weeks that followed. There were moments in the hospital when so much happened at once, I went numb. It was impossible to fully process in the moment, so I’m grateful I had the opportunity to work through some of those feelings before he was born.
In the course of my research I often felt frustrated and even a little resentful that a lot of what I read about early postpartum didn’t apply to me. I knew we’d be in the hospital for an extended stay after surgery, but didn’t know exactly how long. Doctors told me we might get a moment with him before he was whisked to the NICU, but it wasn’t guaranteed. I hoped I could breastfeed, but I knew he had many hurdles to overcome first.
As a soon-to-be first time mom, all these unknowns made it extremely difficult to give into the nesting instinct. What I didn’t know at the time was there is a huge community of heart moms and NICU moms who understood and related to my struggles. I wish I looked up more NICU content, because I would’ve found it much more relevant to me.
In addition to this post, here is another helpful blog about preparing for NICU life. I find all the posts on @dearnicumama Instagram account extremely comforting as well.
What To Pack for Mom
Apologies for the cliche airplane mask reference, but it’s true. You can’t properly care for your child if you don’t care for yourself. It’s likely the last thing you’ll want to do, but start by packing for yourself. Think about what might make you comfortable, knowing you’ll be in a very uncomfortable environment.
I quickly went from a patient in Labor & Delivery to “heart mom” once we walked through the doors at CHLA. On day 1 Jordan tried to get me ibuprofen because I missed a dose during transport and was in a lot of pain. The nurse clearly felt so awkward explaining that no, she couldn’t give me any medication. I was no longer the patient. Oops!
Here’s what I had on hand for myself in my hospital bag. There are so many hospital bag lists available online, so I didn’t go into too many specifics. I mainly wanted to include a few key areas that get overlooked specifically for NICU mamas. Click here for printable version.

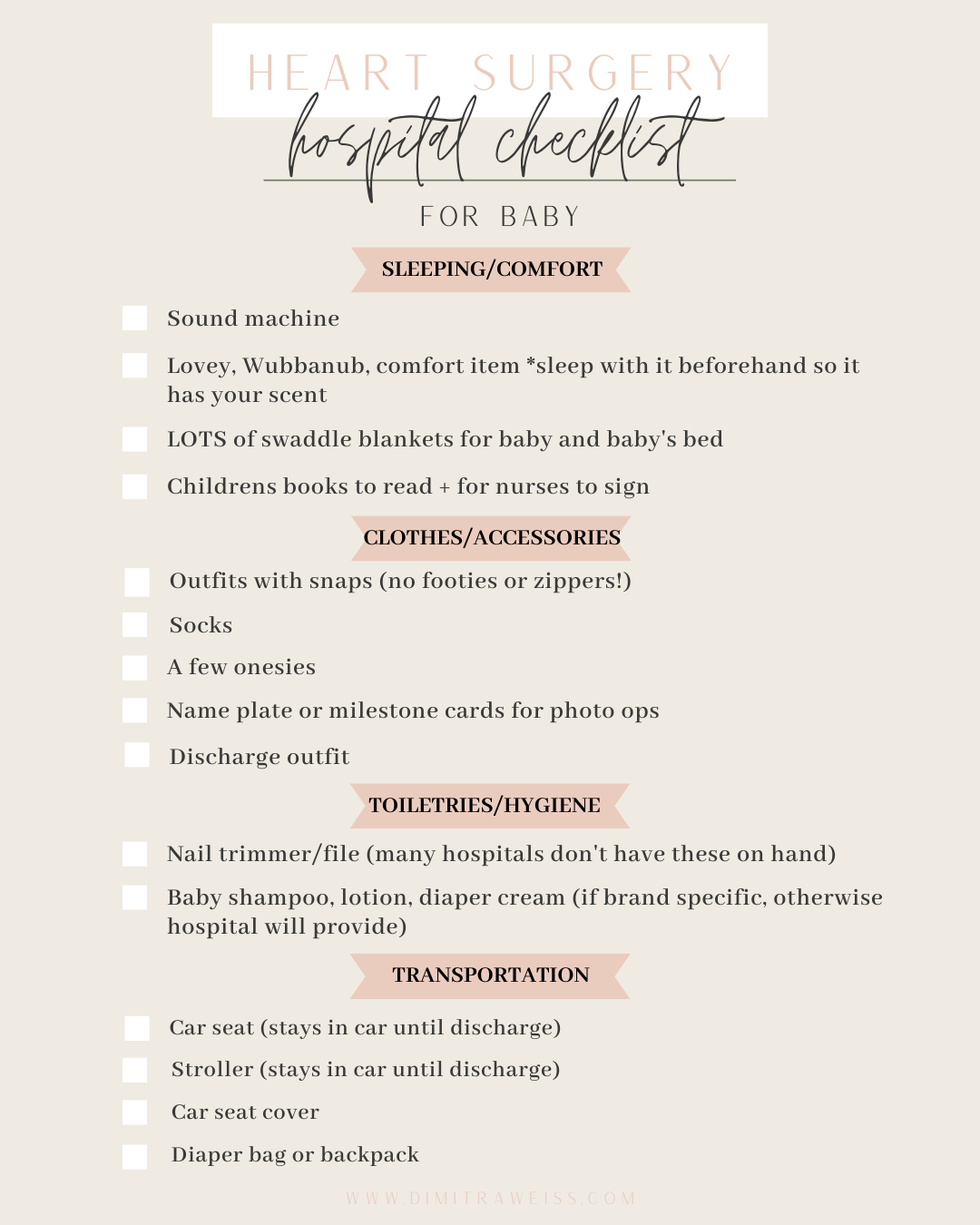
What to Pack for Baby
The reality is your baby will need very little in the hospital. The hospital provides everything imaginable to care for your child before and after surgery. If you don’t see something in your room, chances are someone has access to it elsewhere in the hospital. Everything from toys, books, Mamaroos baby swings, sound machines, etc. It’s all there.
With that said, I’ll never forget the first time a nurse asked if we packed socks. It felt so nice to pull them from my bag and provide for my baby in a way I wasn’t able to in the beginning. Here are a few things I had on hand (that we actually used!) for baby in the hospital. Click here for printable version.
What to Expect in the Hospital After Surgery
Watching your newborn go through open heart surgery leaves a parent feeling incredibly helpless. I’m open about how challenging that part of the experience was on Instagram, but I also want to give parents perspective and maybe even a little bit of hope.
I cried a lot of tears in the hospital and I worried every day. But I also laughed, felt immense gratitude, and fell head over heels for my baby during that hospital stay. We made amazing relationships with his nurses and doctors. We shared stories, had coffee dates and stepped outside for fresh air.
There was a local coffee shop and Mexican restaurant side by side, right around the block from CHLA. We frequented both as an escape. A welcomed distraction if we had to leave the room for a procedure (chest closure, extubation, etc.). Sure, we were dead tired and talked about Leyton 99% of the time. But we still managed to have some really nice moments sitting on those benches.
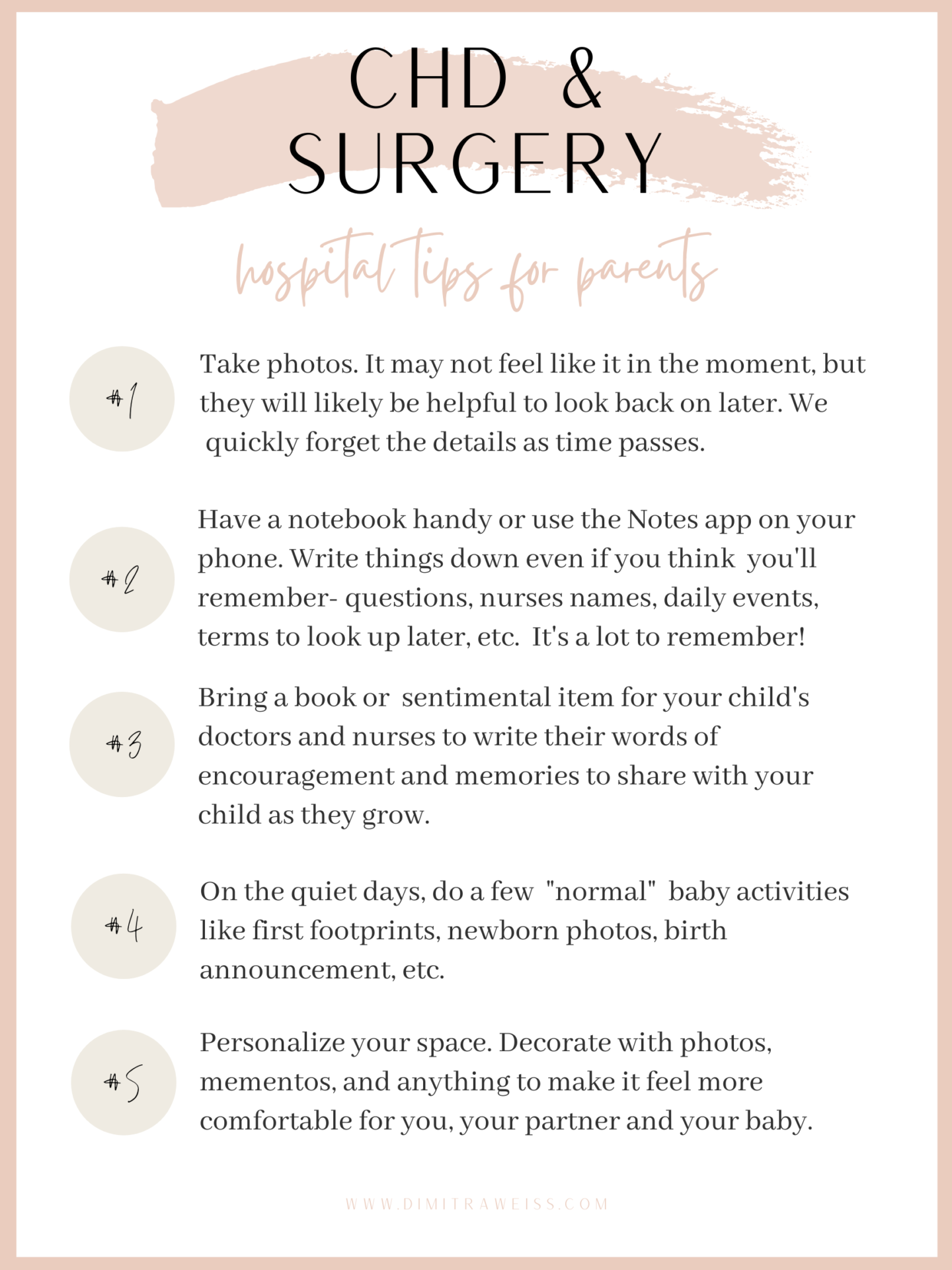
We fell into a daily routine in the hospital, mostly set by the doctors, but it was predictable and comforting. I pumped every 2-3 hours around the clock, so it also helped distinguish day from night!
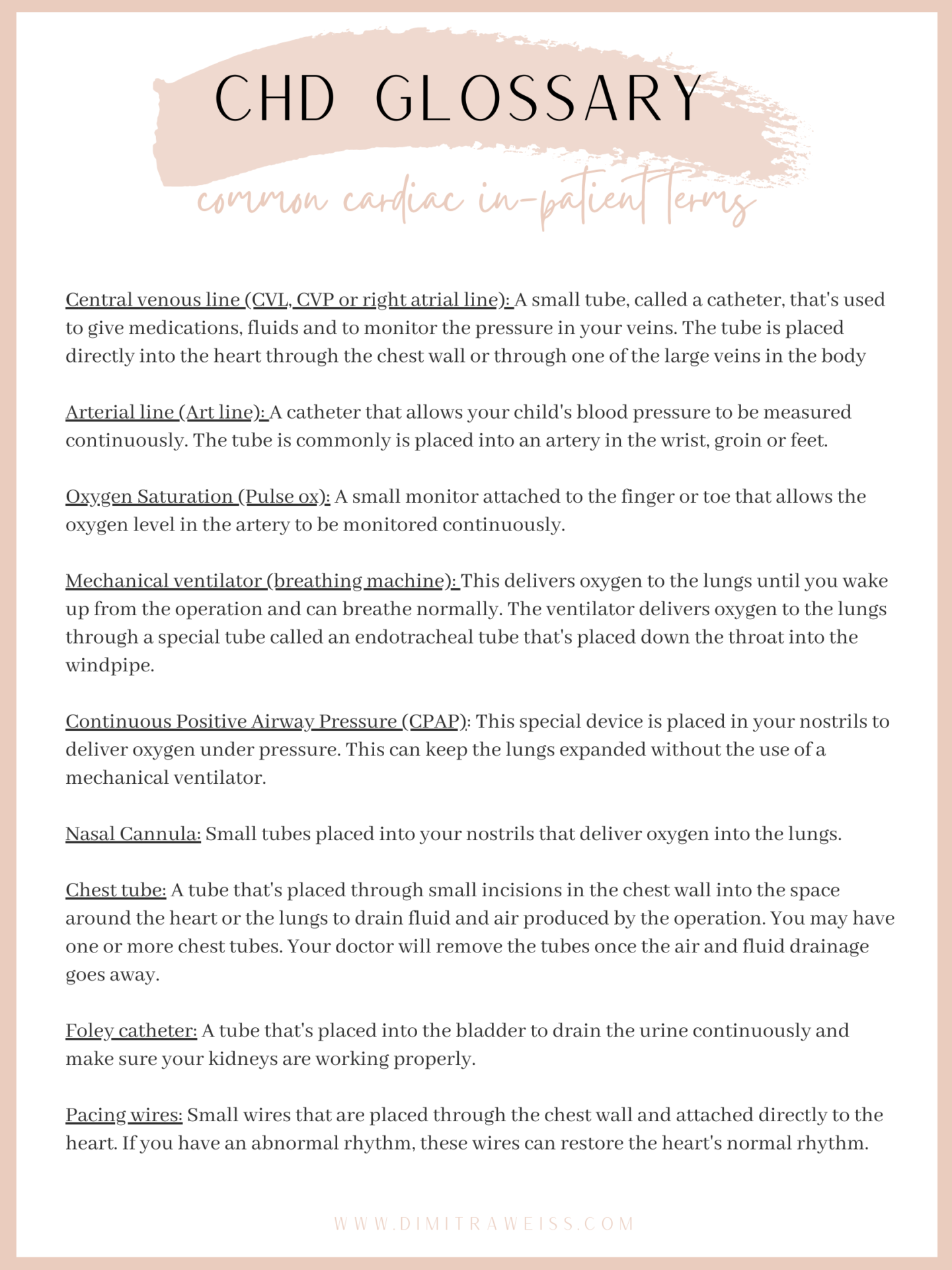
The morning began at 6am to the sound of the x-ray machine wheeling down the hall toward our room. I checked in with the tech while they did exams and vitals, then pumped behind the ugly beige curtain. We greeted our new nurse around 7am and then waited to join his doctors for rounds at 8:30am. After that we went downstairs for coffee and a bite to eat. We also picked up a lot of new lingo throughout our new daily routine.
Here is a list of some common cardiac terms we became familiar with while in-patient after surgery. Click here for a more in depth glossary of cardiac terms.
One of the things I appreciated during our hospital stay was how clearly everyone prioritized Jordan and I as parents. We were immediately given updates and included in care discussions. A few times his doctors pulled us aside to offer further explanation when we overheard something they knew we found alarming. It gave me a sense of confidence that I was well informed without having to hound people down or initiate those conversations on my own.
The nurses also incorporated us into his care, slowly at first. I remember the first time a nurse asked if I wanted to use the sponge to dampen his dry lips and mouth. I beamed like a kindergartener on “Student of the Week Day”! Little opportunities gradually led to us taking over his care completely until the transition to discharge felt smooth and feasible . Don’t get me wrong, it was still terrifying, but we were empowered and excited to embark that next chapter. Plus being nervous is a right of passage for all new parents isn’t it? 😉
FAQ’S
I had a running list of questions about everything relating to Leyton for months. I still do! In the beginning, it was mostly about surgery and his heart, but a lot about general life with him and expectations. It was helpful to keep track and cathartic to write it all down. I saved all my questions on my phone and wanted to list some of them here.
To clarify, these are the questions that came after we asked everything that related specifically to his diagnosis, like expected outcomes/survival rates, etc. These are some of the things you may not think to bring up right away, when all you want to know is, “is my baby going to live?”…
Pregnancy Questions
- Q: Should we do genetic testing or amniocentesis?
- A: This is a personal choice. Based on recommendations from a genetic counselor we did all the in utero genetic testing that was offered to us, including an amniocentisis. This was a stressful decision, and we eventually came to the conclusion that we’ve had enough surprises, the risks were fairly low, and we preferred to be as informed as possible at that point. Everything came back normal for every test. Even my own blood panel that screened for 250+ genetic disorders. I wasn’t a carrier for a single one. d-TGA is very rarely caused by genetic abnormalities and in most cases it’s just how the heart spontaneously forms in utero.
- Q: What caused his CHD? Could I have done something to cause this defect?
- A: I still carry a lot of guilt for Leyton’s CHD, but I’ve been reassured many times it was nothing I did during pregnancy to cause his heart defects.
- Q: What if I deliver early?
- A: The doctors will do everything possible to get the baby as close to full term. It’s ideal if CHD babies meet a weight requirement prior to surgery, however, many CHD babies are born premature and still have positive outcomes. Our cardiologist gave us a 35 week “magic number” to hit and feel confident that the baby would be less likely to suffer complications from being premature. I delivered at 38 weeks with no issues outside his heart.
- Q: Is the baby safe in my stomach?
- A: Yes. It gave me comfort knowing that my body and the placenta provided all the oxygen and nutrients my baby needed to grow, just like any other pregnancy.
Birth/Delivery Questions
- Q: Will I be able to go into labor naturally or will I have to schedule an induction or cesarean?
- A: We had an induction scheduled for 39 weeks because I was due over a holiday weekend and his team was worried critical members might not be on staff when I went into labor. However, I ended up going into labor and delivering naturally a week before that lol. I labored for a long time at home and then the L&D team notified the NICU team when I was finally on my way. I didn’t have to do any of the coordinating while in labor thankfully.
- Q: How many people will be in the delivery room?
- A: This will depend, but typically includes your OB, a few L&D nurses, your support people and the NICU team. In my case it ended up being about 15 people total…not that I noticed lol!
- Q: Can I have a support person in addition to my husband in the delivery room?
- A: This has probably changed due to COVID 🙁 but yes, I was able to have one more person. My husband and mom were both in the delivery room for my son’s birth.
- Q: When can I see my baby in the NICU?
- This depends on many factors, including how stable the baby is, the time of delivery, the method of delivery, if mom is on meds, etc. In our case, Leyton was born late at night and then had a procedure early the next morning so I wasn’t able to get to him until he was about 12 hours old. My husband followed him up to the NICU right away and FaceTimed me in the meantime.
- Q: Will our early separation or the trauma of surgery affect our attachment/bonding?
- A: Nope. Leyton is incredibly attached to me and my husband. I clearly can’t compare our experience to anything else since he is our first baby, but he is the most affectionate and loving child. Our bond continued to deepen and he is easily comforted (for the most part haha) by his father and me.
- Q: Will my child develop a fear of doctors or hospitals?
- Leyton is very aware of these settings, but I wouldn’t say in general he is fearful. When we arrive at appointments he is happy and curious and always greets the nurses with a smile and wave. As he’s gotten older, he’s a lot more resistant to physical exams (temperature, blood pressure, listening to his heart through the stethoscope) and has very little tolerance for longer exams like and echo or EKG, but we’re working on it!
- Q: Will I be able to breastfeed?
- A: Yes! He didn’t feed for the first several days because he was unstable, and didn’t latch until he was almost a MONTH old, but I pumped the entire hospital stay and we worked our way up to exclusively breastfeeding shortly after that. I’m still nursing him once a day at 18 months old!
Hospital Questions
- Q: Will we be able to take tours of the NICU and CTICU ahead of time?
- A: This is different now because of COVID I’m sure 🙁 but yes, we were able to arrange tours of both spaces prior to delivery. It was helpful to get an idea of the environment beforehand, so I really hope something like this is available to parents today.
- Q: Will we have a private room?
- A: Again, this depends on the location, but we did have a private room at both hospitals, with the exception of the NICU. The NICU is set up with 6 babies in each wing with privacy screens around each baby’s bed. We shared a bathroom with our neighbor at Children’s Hospital LA and used the community shower that was available on each floor. Once we were transferred to the step down unit at CHLA we had a private room, bathroom and shower. So luxurious! 😉
- Q: Can we go with him in the transport vehicle?
- A: One of us was able to ride with him during transport so I went in the ambulance and my husband followed in our car with all our belongings.
Surgery and Recovery Questions
- Q: Will he check in with his surgeon post-op? Who follows his care?
- A: We met with the surgeon once before surgery for a meet and greet/Q&A type touch base and then saw him again on the day of surgery, but that was it! He was consulted on every medical decision and a member of the board that decided his plan of care, but we never communicated with him directly. We have a very close relationship with Leyton’s cardiologist and other members of his team, but even though we are forever indebted and very fond of his surgeon, he’s a bit of a stranger to us! I’ve heard this relationship varies depending on the hospital/location, but it’s worth asking who will be your main post-op contact.
- Q: What complications could delay surgery? PPHN- Persistent Pulmonary Hypertension? Other CHD’s?? Premature birth?
- A: This is a bit of an unfair question because the possibilities are somewhat endless. That was a scary thought, so I wrote down every complication I came across, but I actually wish I hadn’t. My son ended up being diagnosed with a second CHD, but it didn’t delay his surgery. It added an extra complex component, but didn’t delay it. Leyton was unstable prior to surgery and it actually caused his team to move his surgery sooner rather than push it.
- Q: What are the risks to his neurological/brain development?
- A: Another somewhat unfair question because yes, CHD babies are at a higher risk for neurological complications due to lack of oxygen, but it’s not something you can easily predict or prepare for. So far we’ve had a few “scares” that led to further testing and all Leyton’s neuro assessments came back normal.
- Q: Typical discharge timelines? When will we receive a discharge date?
- A: This greatly varies. I’ve read stories of some babies going home a week after surgery! Leyton spent 3 weeks in the hospital. We heard the doctors discuss an estimated discharge date at one point, but they pushed it because he was still on oxygen at the time. We had a strong idea we would be going home soon based on the tests they were running in the days leading up to discharge, but we weren’t formally notified until the day of discharge.
- Q: Will he be put on bypass?
- A: Yes. During surgery, the surgeon stopped his heart and put him on a bypass machine while they operated.
- Q: How will we be updated during surgery?
- A: The nurse called us with regular updates and to let us know when Leyton was out of surgery. His surgeon came out and briefly spoke to us afterwards to let us know how the surgery went.
- Q: How long does surgery typically last?
- A: An Arterial Switch Operation typically lasts anywhere from 4-6+ hours including prep and immediate recovery. Leyton’s surgeon had a reputation for working fast and he was out of surgery in under 4 hours.
- Q: When will we be able to see him after surgery?
- A: Typically the surgical team monitors the baby in recovery for about an hour before you can see them. In our case, Leyton suffered a post-op hemorrhage during this time, which resulted in an emergency trip back to the OR. We weren’t able to see him for several hours after, so we were away from him from 8am-8pm. It was a very long day.
- Q: When will we be able to hold him after surgery?
- A: It’s common for babies to come out of surgery with their chest left open due to swelling. This means exactly what it sounds like. A clear bandage covered the open incision. We couldn’t hold him until they closed his chest 3 days after surgery. We were with him at the bedside, held his hand, squeezed his toes and stroked his cheek during that time, but he wasn’t in our arms for several long days.
Aftercare Questions
- Q: How do we care for his incision?
- A: We received full incision care training in the hospital stay so we were well versed by the time we left. The biggest things were keeping it sterile, dry, and not putting pressure on it or the surrounding area. We learned how to pick him up properly, dress him, and give him a sponge bath.
- Q: Will he be able to do tummy time right away? If not, could this effect his head and neck development?
- A: Leyton had sternal precautions after surgery, but they allowed tummy time right away! Regardless, he ended up needing a helmet to correct a severe case of plagiocephaly (flatness of the head) partially due to the few weeks on his back in the hospital. He spent 12 weeks wearing a helmet 23 hours a day. It was a bit inconvenient, but the time flew by and the results were well worth it! I made a whole YouTube video dedicated to our experience with the DocBand helmet if you’re curious to learn more.
- Q: Can we swaddle him?
- A: Yes! Starting right away and even in the hospital. He loved it!
- Q: Do you recommend the Owlet or other at home monitors?
- A: Most medical pros will likely say NO because the Owlet isn’t classified as a medical device. I’ve read it can be prone to false alarms. We bought one anyway thinking the peace of mind would be worth it! By the time we got home my husband and I had PTSD from all the alarms constantly going off in the hospital. We couldn’t bring ourselves to put it on him so it’s still brand new in the box in his closet lol. I know some parents love and swear by their Owlet, and others agree with the scary false alarm claims. I think it’s a personal choice but definitely not a must-have! We learned how to read him and stayed on high alert for red flags whether they were hooked up to a monitor or not.
- Q: How often will we have follow ups?
- This varies greatly from baby to baby, but it will likely start very frequently. It gradually spaced out when he was stable and got a closer together when issues popped up. Leyton started seeing his cardiologist weekly and his pediatrician every two weeks. He also had follow ups with the NICU team, newborn development clinic, and surgical team. Then we went to biweekly cardio and monthly pediatrician. Now he sees his pediatrician every 6 months (on a typical schedule) and his cardiologist last gave a 5 month clearance! A very good sign as to how his heart is holding up.
Conquering CHD has a Guided Questions Tool with more helpful questions for your child’s care provider.
What To Expect During & After Discharge
I mentioned we didn’t get much of a warning before discharge, but we had to check off several boxes before they cleared him to leave the hospital. It’s not uncommon to go home with a feeding tube or oxygen, but his team felt they could safely wean him from both.
The nurses tested us until we proved we knew how to bathe him and care for his incision, prepare his bottle with the appropriate recipe to fortify his feeds, administer his medications and they also gave us an infant CPR course. It sounds like a lot, but you surprisingly have a lot of downtime in the hospital on the good days!
Here’s another list I found in my notes from our final days in the hospital.
Discharge Notes
- CPR Training
- Car seat test – two hours strapped in the car seat with no oxygen desaturations
- Post-Recovery
- Sternal precautions – no armpit hold
- Incision care – methodical cleaning, keep dry, do not submerge in water
- Immune suppression – extra precaution not to get sick! Synagis vaccine for RSV
- Developmental delays are more common in heart kids, good to follow and watch for missed milestones
- Putting on weight – Important to make sure he stays on his growth chart
- Endocarditis/Dentist Appointments – he needs antibiotics before dental appointments (even a cleaning!) to prevent risk of infection getting to his heart
- Clinic/follow ups – so. many. follow ups. 🙂
My hope for this blog post was to collect resources that are easy access for newly diagnosed parents. It’s not meant to add stress. It’s good to know but I assure you, none of it was in the forefront of my mind. Once we got home I mainly focused on the unencumbered snuggles, sleep deprivation (lol) and staring in awe of my perfect baby. Sometimes thinking too far into the future leads to an anxiety inducing trail of thoughts. (Even for me a year and a half out!) I don’t want to add to that with any of these notes.
This post will always be here to refer back to if it’s too much to take in right now. I get it. It’s a lot! I’m also always just a dm or email away, as are MANY other CHD parents.

