Breathing Episode | NG Tube | Post-Op Oxygen Support
I intended to finish Leyton’s post-op story in one more post, but after looking back at my notes, there’s still so much I don’t want to forget. My mind often drifts to the memories of his open heart surgery to repair two CHD’s; Transposition of the Great Arteries (TGA) and Coarctation of the Aorta (COA). Writing it out is a cathartic release, so I’d like to share a few more posts before moving on to real time updates. Click here to start from the beginning and jump back to his diagnosis.
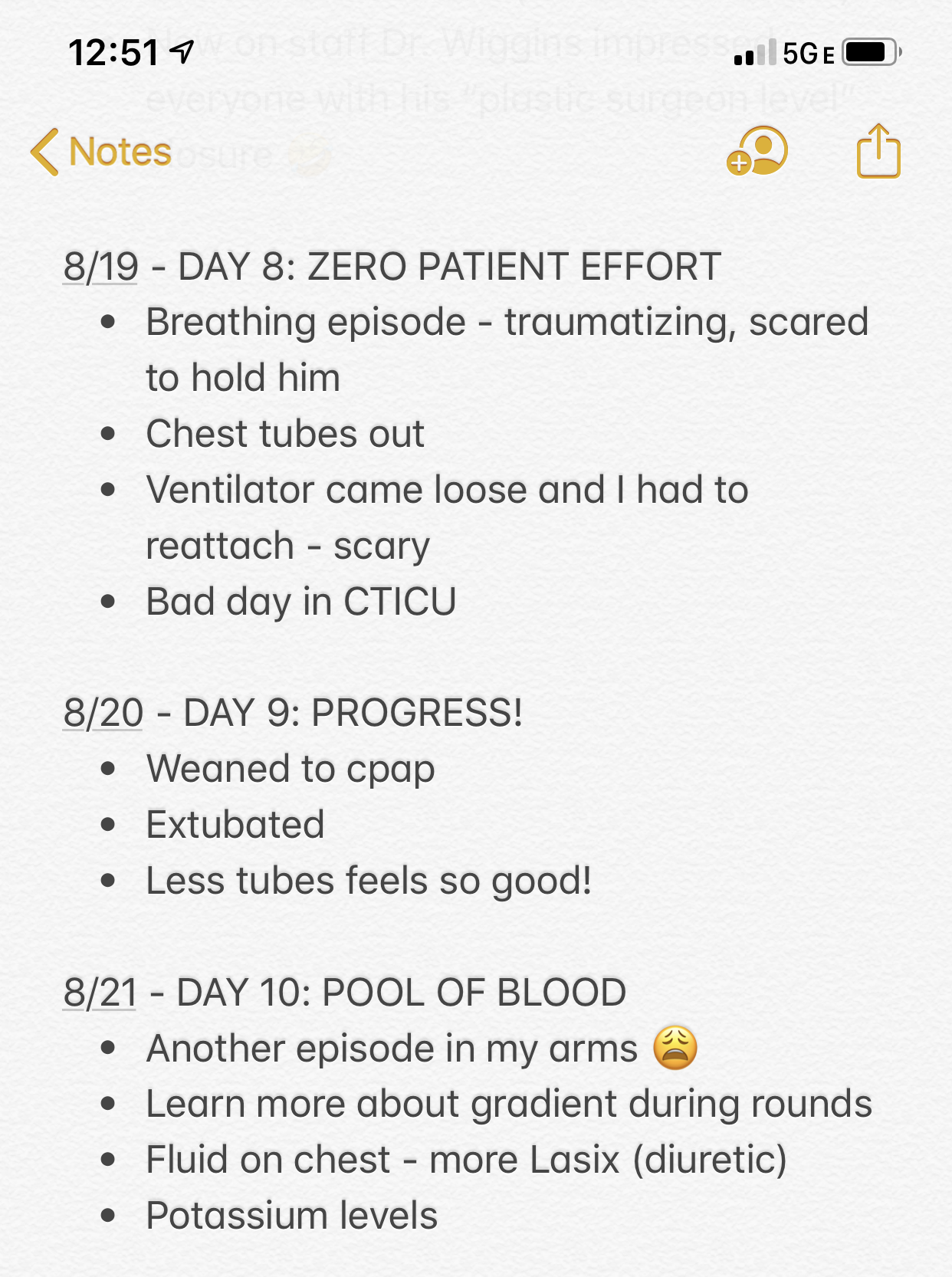
If we learned anything in the post-op period, it’s that recovery is not linear. The days are long and grueling even when they’re trending upward. There are bound to be post-op hurdles, even in the most straightforward TGA cases.

As a parent, each hurdle felt insurmountable. Some days it seemed like we took 3 steps forward only to take 2 steps back. He made progress, but we occasionally lost sight of it in the midst of setbacks and new developments.
Leyton’s two biggest post-op obstacles were breathing and feeding without medical support. Obviously these were crucial to thrive, but they also required an incredible amount of effort for a baby his size. He tired easily and sometimes burned more calories than he consumed in a single feeding. Healthy heart function pumps oxygen to the body, so keeping his oxygen levels in an optimal range was a big concern as well.
Breathing
Leyton was intubated for five days after surgery. He generally required quite a bit of oxygen support and had a few scary episodes while on the ventilator. The first two occurred while he was in the NICU so I was only told about them after the fact, but I’ll never forget the one he had in my arms.
We went several long days without holding him right after surgery while his chest was left open. After his chest closure, I made up for lost time and held him for hours each day. One night he was particularly alert. I spoke and sang to him while he just gazed up at me. Talk about BLISS for a new mom.
Suddenly out of nowhere his eyes rolled back and he went completely limp in my arms. I shook him and called his name, but he didn’t respond. The alarms were blaring. When I looked up at the monitor the words “ZERO PATIENT EFFORT” were flashing over and over.

In a panic Jordan jumped up to call for Leyton’s nurse, but she was already running down the hall toward our room. Two other nurses and a respiratory therapist ran in as well. She scooped him out of my arms and placed him back in his isolette.
It was probably only a minute or so, but time stood still. It felt like an out of body experience. I could see the commotion right in front of me, yet felt completely removed and numb at the same time. I imagine it like being deep underwater where it’s silent and knowing waves are crashing above you at the surface.
Leyton eventually came to. They ran tests, checked all his vitals and ultimately assured us he was fine. The nurse said she didn’t know what happened, but it was possible he was comforted in my arms and his heart rate just dropped. I was terrified to hold or even go near him for the rest of the night.
Two days later, I was holding him again and felt something warm under my elbow. I picked him up and saw a giant pool of blood soaked through the pillow supporting his head. I remember being startled and confused because he looked completely fine. The nurse said it was coming from the central line (CVC) in his neck. She flushed it and, again told us he was fine. That didn’t stop me from feeling guilty that the scariest incidents only seemed to happen when he was in my arms. 🙁
They successfully extubated him and weaned to CPAP at 5 days post-op. He still needed a lot of help breathing, but we knew it was a step in the right direction. Plus he looked so much more comfortable without all the extra tubing.

Ultimately it took him another two weeks to wean off oxygen all together. As much as I wish I had the utmost faith that he would breathe on his own when he was ready, I admit there was a huge part of me that doubted the day would come. He was on a high flow nasal cannula for weeks, and then eventually just a “whiff” of oxygen.
His nurses did trials several times a day. Each time they turned off his oxygen he desatted immediately, forcing them to turn it right back on. This went on for days. I remember accepting the possibility he may go home on oxygen and trying to picture what it would be like to manage ourselves.
Then one day – poof. His nurse cranked it off and his oxygen levels stayed in the 90’s from that moment on. An hour went by, then three, then halfway through the day we trusted that he would actually go home tube free!
Feeding
Speaking of tubes…Leyton had an NG tube placed after surgery, which is not uncommon for CHD babes post-op. An NG tube is a small tube inserted through his nose and into his stomach which supplies nutrition.
For 12 hours prior to any procedure his team withheld all feeds. Given the timing of his balloon procedure, then surgery and finally chest closure, his only nutrition until he was 5 days old was IV fluids. Then we fed him tiny amounts of my pumped colostrum through the feeding tube. The nurses showed us how to do it and we were so grateful to get to participate in his care that way.

It took several days before he was strong enough to try feeds from a bottle. Even after we introduced bottles the feeding tube stayed in place so we could use it to finish a feed through the tube if he got too tired on the bottle.
I asked every day if we could try breastfeeding, but the doctors and nutritionist agreed we had to wait until he was stronger. I desperately wanted to nurse him and felt like every day that passed, our chances of successfully breastfeeding slipped that much further away. (Thankfully, I couldn’t have been more wrong about that!)
His team wanted him to take three consecutive full feeds from the bottle before they felt comfortable removing the NG tube. Once he got the hang of it, he rocked it. Removing the tube felt like a huge victory and earned us a ticket out of the CTICU!
From there we moved to CHLA’s step down unit, called CVAcute. I’ll share what leg of the journey brought in my next post. 🙂

